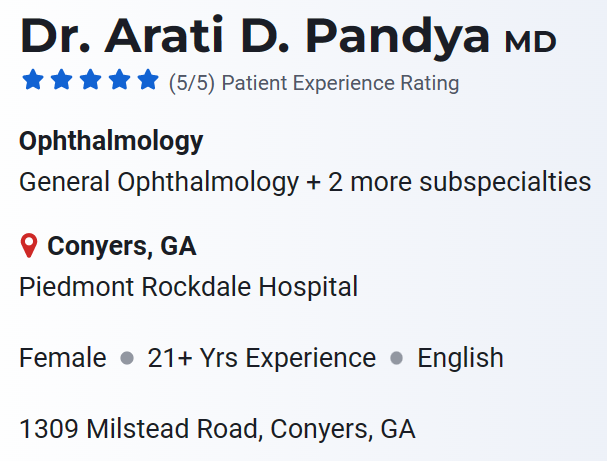
The lawsuit filed against ophthalmologist Dr. Aarti Pandya

Do you know what an ophthalmologist does? An ophthalmologist is a full-fledged medical doctor, even though they can both recommend corrective eyeglasses and provide eye exams.
An ophthalmologist can make diagnoses, give prescriptions, do surgery, and even carry out research. The majority of these medical experts continue to polish their skills in a certain specialty, either by mastering a technique or therapy or by learning everything they can about a specific component of the eye, such the cornea or retina.

Aarti Pandya, the M.D of Pandya Practice Group offers cutting-edge surgery and medicinal treatments for prevalent eye conditions such as dry eye, glaucoma, cataracts, age-related macular degeneration, and refractive errors. Her patients’ attainment and maintenance of good eye health is something she claims herself as a good doctor.
Settle down the allegation
She has agreed to pay about $1,850,000 to settle allegations that they broke the False Claims Act by, among other things, billing the government for cataract operations and diagnostic tests that weren’t actually necessary for patients, tests that were insufficient or of no use, and appointments that didn’t offer the level of service promised.
U.S. Attorney Ryan K. Buchanan stated, “Physicians who perform procedures and tests without a valid medical need prioritize profits over patients and expose those in need to needless risk.” “Our office is committed to enforcing responsibility for doctors who expose people to unnecessary medical care and waste taxpayer funds,” the agreement reads.
According to Keri Farley, special agent in charge of FBI Atlanta, “We must reassure consumers and taxpayers that medical needs, not fiscal greed determine healthcare.” “This settlement should serve as a reminder that the FBI will not tolerate healthcare providers who engage in schemes that defraud the industry and endanger honest patients,” the FBI stated in a statement regarding the agreement to settle.
The medical suitability of the services clients require to preserve their health should be taken into consideration in the first place when coordinating care for recipients, according to Special Agent in Charge Tamala E. The opposite of good medical treatment is putting people through unnecessary procedures only to take advantage of the healthcare systems they rely on. The HHS-OIG and our judicial partners are committed to looking into service providers who may endanger patient safety and the integrity of the federal healthcare system.
Defense Criminal Investigative Service (DCIS), Southeast Field Office Special Agent in Charge Darrin K. Jones, stated, “We are committed to fully investigating those who fraudulently bill the Department of Defense (DoD) health care system to benefit their own financial gain at the expense of service members and their loved ones.” We appreciate the commitment to defending America’s warfighters shown by the U.S. Attorney’s Office and our investigative partners.
This agreement resolves charges that Aarti Pandya intentionally filed fraudulent claims for YAG laser capsulotomies and medically unnecessary cataract extraction procedures with federal healthcare programs from January 1, 2011, to December 31, 2016.
According to acknowledged medical practice norms, Aarti Pandya was accused by the authorities of performing these treatments on patients who weren’t eligible for them and, in some circumstances, injuring her patients. The government also claimed that Pandya gave bogus diagnoses of glaucoma to patients in order to support pointless diagnostic procedures and treatments that were charged to Medicare.
Many of the diagnostic tests that Pandya requested, according to the government, were either improperly carried out, carried out on malfunctioning equipment, or were not interpreted in the patient’s medical file as required by Medicare.
In accordance with the FCA’s qui tam, or whistleblower, procedures, this payment settles claims made in a complaint brought by Laura Dildine, a former Pandya Practice Group worker. The FCA permits individuals to file claims against deceptive claims on the government’s behalf and participate in the proceeds. United States ex rel. Dildine v. Aarti D. Pandya, M.D. et al., No. 1:13-CV-3336-LMM, is the name of the lawsuit, which was filed in the northernmost district of Georgia. In 2018, the United States entered as a party to this litigation.
The Pandya Practice Group was denied payment from Medicare for Part B claims after the government interfered in the qui tam lawsuit, according to HHS. On October 23, 2019, the payment suspension was put into place.
Aarti Pandya and the Pandya Practice Group unsuccessfully contested the payment suspension in the district court. The Pandya Practice Group consented to forfeit the suspension sum to the government as part of the resolution of the claims made by the government in this case. As part of the agreement, the payment suspension will be lifted.
Aarti Pandya and the Pandya Practice Group have contracted with OIG under a comprehensive, multi-year Integrity Agreement and Conditional Exclusion Release (IA) that is more stringent than OIG’s normal agreement in order to safeguard federal health care programs and beneficiaries moving forward. In addition to strengthened material breach penalties, the IA incorporates training and reporting obligations.
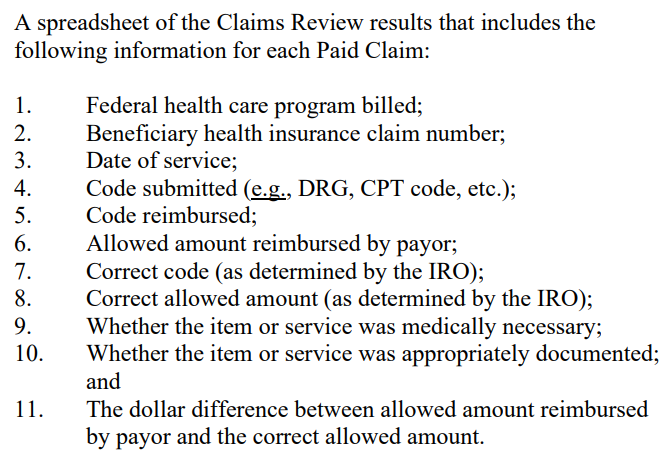
The IA also mandates that Aarti Pandya and the Pandya Practice Group work with an Independent Review Organization to review claims on a yearly basis to check for medical necessity, proper documentation, proper coding, submission, and reimbursement of the goods and services provided. OIG did not relinquish its permissive exclusion power, and it won’t do so until Aarti Pandya and the Pandya Practice Group have complied with the IA’s requirements.
Assistant US Attorneys David A. O’Neal, Austin M. Hall, and Akash Desai were in charge of the probe of this case as well as the legal action taken against Aarti Pandya, MD, and the Pandya Practice Group. There has been no judgment of responsibility with regard to the claims addressed by the agreement; they are only accusations.
The Bottom Line
The 100 Medicare-paid claims and 100 Medicare-paid claims from managed care are to be randomly chosen by the IRO (referred to as “Claims Review Samples”) as a sample. The IRO must review the Paid Claims in light of Dr. Aarti Pandya’s documentation and the requirements of the relevant Medicare and Medicare-handled care programs to ascertain whether the goods and services provided were legally required and properly documented as well as whether the claim was properly coded, uploaded, and refunded.






